Abstract
There is no established treatment for patients unresponsive to first line therapy for chronic graft versus host disease (cGVHD). Infusion of mesenchymal stromal cells (MSCs) is a promising alternative in this situation, but the treatment efficacy and mechanism of action have not yet been established. Furthermore, there is great need for biomarkers for selecting patients that are more likely to respond to MSC therapy.
In this study, 11 patients with severe steroid-refractory (SR) cGVHD were treated with repeated infusions of MSCs. The treatment consisted of 6 to 9 infusions (once every month) of 2x106 allogeneic bone marrow MSCs/kg. Clinical response was evaluated using the National Institutes of Health (NIH) criteria. Blood samples were taken before, and at several time points shortly after each infusion. Immunophenotyping and cytokine analysis were conducted by flow cytometry, ELISA and multiplex analyses.
Nine patients completed the treatment and were evaluable for response. By the end of the treatment, six patients had responded to MSC therapy according to NIH criteria. Further, five of the six responders showed durable improvement at final evaluation, 12 months after finishing MSC treatment.
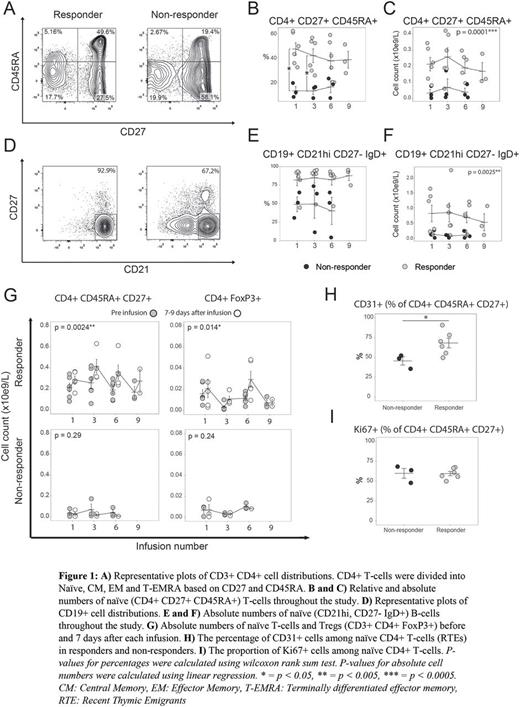
First, we investigated whether there was a difference in the immune cell distribution between the responders and the non-responders before and during MSC infusions. We observed significantly higher numbers of naive T helper (Th) cells and naïve B cells prior to the treatment in the responders compared to the non-responders (fig. 1 A-F). These differences remained unchanged throughout the treatment. Further, we found that in the responders, naïve Th cell numbers (fig. 1G), regulatory T-cells (Tregs, fig. 1G) and immature NK-cells, but not B-cells increased within 7 days after each MSC infusion. No such increases were seen in the non-responders. By the next infusion, the levels returned back to baseline. Tregs were divided into CD45RA+ FoxP3low "naïve Tregs", CD45RA- FoxP3hi "activated Tregs" and CD45RA- FoxP3low "non-Tregs" (Miyara et al., Immunity 2009). The responders had a higher proportion of "naïve Tregs", while the non-responders had a higher proportion of "non-Tregs", among total Tregs.
Next, we asked whether the striking differences in naïve T cell numbers and the observed short term increases after MSC infusion were due to mobilisation from the thymus, or due to proliferation of the existing circulating pool. The proportion of Ki67+ Th cells was similar in the responders and non-responders (fig. 1I), indicating that the mechanism was not increased proliferation. Instead, there was a significant difference in the percentage of recent thymic emigrants in naïve Th-cells suggesting a better thymic function in the responders (fig. 1H).
To conclude, in our study, MSC treatment was able to induce durable responses in patients with severe refractory cGvHD. Further, our data suggest that success of MSC treatment for patients with refractory cGvHD is dependent on the immunological characteristics of the individual patient. More specifically, we propose that sufficient thymic function, generating sufficient numbers of naïve T-cells and naïve Tregs, is required for responsiveness to MSC treatment in these patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal